The Front Lines
Peter H. Kilmarx ’83, DMS’90
Deputy Director, Fogarty International Center, U.S. National Institutes of Health (NIH)
Bethesda, Maryland
Kilmarx does not flinch from disease. While serving in the Peace Corps from 1984 to 1986 in what’s now the Democratic Republic of Congo, he suffered from bouts of malaria every few months. In 2009, when his wife contracted H1N1, Kilmarx took care of her at home. In 2014, he toughed it out in Sierra Leone during its brutal Ebola outbreak as the response-team leader for the Centers for Disease Control (CDC). Today, Kilmarx helps coordinate international coronavirus research and is hopeful about an NIH-funded Phase 1 trial with human volunteers that began in Seattle in March.
If Kilmarx is unflappable, it may be no surprise he admires boldness in others. China’s response to Covid-19, he says, was “just remarkable.” Wuhan, the ground zero of the pandemic, benefited from 1,800 teams of epidemiologists tracking the virus, plus a new hospital that was constructed in less than two weeks. South Korea, he says, deserves credit for mining the phone records of victims to retrace their steps and determine such granular detail as their seats in theaters. The data was shared with the public so people could see if they’d crossed paths with the infected. “You could do a robust response like this in a wired and moderately authoritarian society,” Kilmarx says. “It would be a challenge in a federation like the United States.”
Well-versed and deeply prepared—back in February Kilmarx bought boxes of plastic gloves while urging friends to make sure their home Internet connections were up to speed—the director is also just another civilian trying to stay safe. When ordering takeout to his Maryland home in March, he asked that it be left on the steps. He wore gloves to unpack it and rinsed the containers with soap.
Clinton White ’77
Professor, Infectious Disease
University of Texas Medical Branch (UTMB)
Galveston, Texas
From his window, White has a clear view of Galveston National Lab, whose mundane, office-building appearance seems at odds with what goes on inside. The structure—the only one of its type at a university hospital—contains a biocontainment facility where experts study deadly pathogens. The proximity of the lab, which in 2014 worked on an Ebola vaccine, has upsides: It’s stocked with hard-to-find testing equipment. Though Galveston has been relatively unscathed by Covid-19, the supplies have allowed those in the area who need tests to get them.
White isn’t surprised the lab is well supplied. “The business principle that keeps warehouses lean, like Amazon’s, it’s the same with hospitals. They don’t keep stores of masks and ventilators to lower costs,” he says, “but there are societal benefits to avoiding a lean supply chain.”
Galveston may not be a corona hot spot, but it does have infected pockets, such as Hospital Galveston Unit, a prison for which UTMB provides care. When White spoke with DAM, nine prisoners were being treated in one section of the facility; another three were convalescing in a converted operating room. White expected the situation to worsen there, as employees seemed to be spreading the virus: “Prisons are not set up to socially distance people. Prisoners are isolated from society but not from each other.”
White’s hospital is also one of the sites for trials of remdesivir, an experimental, intravenous anti-viral recovery drug from Gilead Sciences that had early signs of success but whose efficacy has been questioned. “It seems to have better results than hydroxychloroquine, which in some cases,” White says, “can be worse than the disease itself.”
Margaret “Maggie” Feeney ’92
Professor/Chief, Pediatric Infectious Diseases and Global Health, UCSF School of Medicine/UCSF Benioff Children’s Hospital
San Francisco
For Feeney, the pandemic served up a triple challenge: dealing with the shutdown of her lab (later reopened as essential because of its study of mother-to-child disease transmission), physical limitations on her ability to care for young patients, and having her 7-year-old twins at home instead of in school.
Feeney is pleased with the effectiveness of her hospital’s “successful transition to telemedicine,” which, in some cases, she says, has been as good as seeing patients face to face. She also considers herself fortunate to work in San Francisco. “I can’t say enough positive things about the exemplary way the Bay Area has dealt with the pandemic,” especially the speed with which stay-at-home orders were issued, Feeney says. “It’s incredible the way people have rallied together and stepped up.”
In her lab, researchers study blood samples from mothers and infants to learn if fetal transmission from a mother to her fetus occurs and how infants respond immunologically. “We can be informed about how to proceed in the future by learning why children seem to be less affected by the virus,” she says. She has consulted on cases of children who were infected and says much more has to be learned about underlying risk factors.
Reflecting on her experience in the first weeks of the pandemic, she can’t forget one patient in the bone marrow transplant unit at UCSF whose mother had two other children at home. “That mother was trying to trade off time between her children even as her police officer husband responded to 911 calls between his own parenting shifts. That is the reality,” Feeney says.
Martin S. Cetron ’81
Director, Global Migration and Quarantine
Centers for Disease Control and Prevention
Atlanta
“If you don’t have an appropriate amount of humility and fear, then you have lost a healthy amount of respect for the power of Mother Nature,” says Cetron, a pandemic expert who coauthored a 2007 CDC paper that may have introduced the now-ubiquitous concept “flatten the curve.” Cetron, an infectious disease doctor and Emory professor, modestly declines credit—“This is not a me moment, this is a we moment,” he says—but the paper spells out the critical importance of social distancing to slow a disease’s spread to buy time to prepare, avoid hospital overcrowding, and reduce the total numbers of cases and deaths. Origins of the guidance to simultaneously shutter public spaces, impose social distancing, and isolate the sick might be surprising. Cetron and his team dug into newspaper archives and studied reports about 43 American cities during the 1918 influenza to see which policies worked and which did not. Cross-referencing school, theater, and church closings with death counts, Cetron found that cities such as St. Louis, which imposed a mass shutdown, cut losses far better than, say, Philadelphia, where a World War I-themed September parade so sickened the crowds that every hospital bed in the city was filled within three days.
“It’s really too late to act when you’re already piling up bodies like cordwood, as some of the newspapers back then would say,” says Cetron, a member of the Dickey Center board of overseers and frequent lecturer at Geisel Medical School. He was in Hanover when he learned of the viral outbreak in China and raced back to Atlanta. Working 18-hour days and focused on the here and now, Cetron suggests that handshakes might not survive the current crisis. Perhaps, Cetron says, people can greet each other with their arms crossed on their chests, like the “Wakanda forever” salute from the Black Panther film.
Jaimie (Paul) Meyer ’00
Infectious Disease Physician/Assistant Professor of Medicine, Yale Medicine/Yale School of Medicine
New Haven, Connecticut
With a practice populated by HIV patients and women returning home from prison, Meyer is used to challenges, but Covid-19 “turned our world upside down,” she says. As of mid-April, Yale New Haven Health (which operates four hospitals in southern Connecticut and one in western Rhode Island) had almost 600 Covid-19 patients, roughly half of them in New Haven. A month earlier, when the virus appeared in Connecticut following a much-publicized party in Westport, Yale New Haven Health installed a Covid-19 call center and transformed its consulting model from in-person visits to telemedicine.
Previously focused much of the time on clinical trials, Meyer began manning the hotline, which was receiving thousands of calls a day—sometimes from clinicians and patients as far away as Tanzania—and consulting remotely not only on clinical care, but also on “de-carcerating” prisoners at high risk of infection. Given its nature, her work has always extended beyond clinical care into advocating for patients and trying to inform public and health policy. “But not to this degree,” she says. “When you live under this big red dot that represents cases in our part of the country on a national map, everything feels different.”
The Yale hotline was particularly instructive: “Day One we had people from the [Westport] party calling; Day Three it was family members; Day Five it was neighbors; Day Seven the schools closed. Day One we had 371 calls; one week later we had more than 2,400. You could just watch the virus balloon out.”
As stressful as the overload of patients and callers has been, Meyer remains buoyed by her colleagues. She found “cathartic” an evening Zoom book group discussion with fellow members of Yale’s infectious disease department. The book they had hastily agreed to read? Camus’ The Plague. “It was amazingly relevant as it raises issues of denial from government, pathos, feelings of despair but also heroism and humanity.”
Daniel Lucey ’77, DMS’81
Senior Scholar, O’Neill Institute for National and Global Health Law, Georgetown Law
Washington, D.C.
You name it, Lucey has seen it. He’s been a leading researcher of diseases including HIV, anthrax, SARS, MERS, Ebola, Zika, yellow fever, influenza, and plague. After reading a December 30, 2019, posting from the Hong Kong health department about unexplained pneumonia cases in Wuhan, China, he wanted to get there but was forced to settle for Hong Kong in February. He says the coronavirus is like nothing he’s seen before.
“The United States has a structure in place that could have been sufficient to deal with Covid-19,” he says. “But equally important are the people populating the structure. There is a tendency in the United States to believe in the government. I’d like to think that if someone with responsibility for monitoring the national stockpile [of medical supplies] told people in Congress there were no masks because the money had been spent on small pox vaccine, someone would have said, ‘That’s a false dichotomy. We need both.’ ”
Proof of Lucey’s prescience can be seen at the Smithsonian National Museum of Natural History in Washington, D.C., when it reopens. “Outbreak: Epidemics in a Connected World” has been on display for two years. Organized in conjunction with a Smithsonian anthropologist, it highlights animal-to-human pandemics and how to combat them. The final plaque quotes Lucey from years earlier: “What’s next is already here. We just haven’t recognized it yet.”
The 300 people at the exhibit’s opening, Lucey acknowledges, included some top people from the NIH, CDC, U.S. Department of Health and Human Services, and FDA, but he received no calls from attendees asking how best to prepare for the next pandemic, something on which many of them were working. The focus of their organizations was primarily on influenza, not on a new coronavirus, Lucey says.
His discussions with colleagues in Hong Kong and Singapore has led him to question the alleged source of the coronavirus outbreak in Wuhan late last year. “I think this virus emerged as early as September as a naturally occurring spillover event from a still-unknown animal species into our human species—and certainly not in December in the Wuhan wet market,” he says.
Douglas White ’95
Critical Care Physician/Ethicist/Professor
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania
White has made end-of-life decisions, specifically those made in ICUs, a focus of his research. Collaborating with legal and medical scholars and philosophers, he coauthored “A Framework for Rationing Ventilators and Critical Care Beds During the Covid-19 Pandemic” in the March 27 online edition of the Journal of the American Medical Association, as well as the University of Pittsburgh white paper published in April, “A Model Hospital Policy for Allocating Scarce Critical Care Resources.” The papers set forth protocols already adopted by the states of Pennsylvania, Massachusetts, Colorado, several hundred U.S. hospitals—including Dartmouth-Hitchcock—and health systems from South Africa to New Zealand to Mexico. “The reaction has been overwhelming,” he says.
White’s recommendations, known as “The Pittsburgh Model” and to be used only in national emergencies, put decision-making in the hands of a triage team headed by a triage officer who can be objective when reviewing competing demands of physicians and provide clear criteria for ICU admission, ventilation, and reassessment of continued critical care. “Race, ethnicity, and socioeconomic status should not factor at all into triage decisions, nor should any predictions about long-term life expectancy,” he says, “because that can be affected by things like low socioeconomic status, poor access to healthcare and healthy food, and dangerous living situations.”
As for the wisdom of medicine being regulated at the state level in the United States, White acknowledges, “Having guidance from the federal government would give you consistency at the expense of states’ rights, which goes against foundational principles of U.S. governance structure. There are a handful of states that don’t give any guidance and, equally important, others that give problematic guidance that discriminates against individuals with disabilities. I started this work more than a decade ago after engaging unsuccessfully with states and groups with that kind of baked-in discrimination that weren’t willing to change.”
White also advocates for legal immunity for those doctors who make life-and-death decisions when they are following sound state guidelines.
Peter F. Wright ’64, DMS’65
Specialist, Infectious Disease and International Health, Dartmouth-Hitchcock Medical Center
Lebanon, New Hampshire
The face of the battle against the coronavirus may be doctors hooking patients to ventilators in isolation wards, but a deep bench of behind-the-scenes players is performing research that may be just as critical. Toiling daily in a lab on a floor that’s been mostly empty for weeks because of a work-from-home order, Wright studies blood from a half-dozen Covid-19 survivors to learn how their antibodies behave. “A question we are very interested in is, if you get the disease, do you become immune?” he says.
Wright, working with doctors elsewhere, wants to learn precisely how the antibodies destroy protein spikes, those wine-colored bumps on the surface of the virus in that ubiquitous illustration that makes the virus resemble a forested planet. The spikes hook into lung cells, allowing the virus to take root. The researchers’ data may impact NIH efforts to develop its vaccine. “We think the trial is very relevant,” Wright says, “and is moving forward well.”
Wright, who did his residency and fellowship at Boston Children’s Hospital and teaches pediatrics at Geisel, is curious why kids seem to have lower death rates than adults when it comes to Covid-19. He has been aware for many years how quickly diseases can ravage a country. Since the 1970s he has volunteered his services in Haiti as it has struggled with cholera outbreaks. “A colleague told me I would learn more about infectious disease in two months in Haiti than in the rest of my fellowship,” he says, “and he was right.”
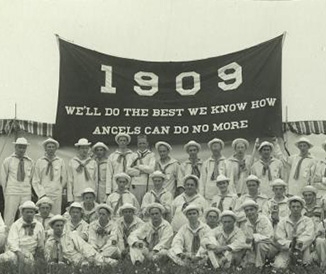
But America has hardly been immune, and anyone who has paid attention to previous outbreaks, such as H1N1 in 2009, should realize this country is vulnerable, he says. “I think this was all somewhat inevitable.”
Rachel Bender Ignacio ’04
Physician-Scientist/Assistant Professor in Infectious Diseases/ Associate Director, AIDS Clinical Trials Unit, University of Washington
Seattle
Like many HIV researchers, Ignacio has seen her research “back-burnered” by the frantic search for therapeutic treatment of Covid-19 patients. “We’re talking about the same communities being most affected,” she says. “Those where people disproportionately work in public transportation, gig economy, day labor, manufacturing, and other jobs where they have less ability to stay home and higher risks of job loss. As people in the communities I serve say, ‘We’ve been here before.’ They are rallying to be sure that Asians aren’t stigmatized and to take up the advocacy piece of the fight.”
There are no treatment “magic bullets,” says Ignacio. “Studies in Europe and China hint that a few FDA-approved drugs may be effective. Due to the urgency of the pandemic and hype in both the press and scientific communities, we have put clinical practice before evidence. The trials I am involved in are double-blind, randomized, controlled trials that will be analyzed by expert statisticians. This is mandatory before we can say that any of these therapies work.
“One hundred percent of infectious disease doctors and epidemiologists anticipated an international epidemic, if not possible global pandemic, on the order of Covid-19,” she says. “It was keeping us up nights as soon as news from Wuhan broke, so it was very frustrating to see at the national level a political rather than preparedness response. Only in the United States is there a perceived conflict between individual liberty and the provision of universal healthcare, a disconnect when it comes to social justice. I hope people will think very seriously about the ramifications of this pandemic on social disparities and on our public health infrastructure when they vote. We need to protect the safety of our elections and fight for mail-in ballots in all states.”
Norman Moore ’88
Director, Global Infectious Diseases, Abbott
Scarborough, Maine
“If you love things that are black and white, you can go into chemistry or physics,” says microbiologist Moore. “I love microbiology because it’s gray and filled with ‘what ifs.’ Viruses don’t like playing by the rules. There’s so much that changes, there’s always a new one.”
As he prepared to turn 50, however, Moore was determined to do something decidedly non-science. “As I told my wife, it’s going to be less expensive than me buying a sports car to celebrate my mid-life crisis,” he says. Instead he wrote a humorous book, If I’m the King of My Castle, Then Why Am I Holding a Dirty Diaper? (2015). Little did Moore realize, despite holding eight U.S. and 39 international patents including tests for Legionnaires’ disease and pneumonia, that five years later he’d be dealing with the biggest crisis in modern history.
Moore, who earned a Ph.D. from the University of New Hampshire in 1994, travels frequently to lecture at conferences about best practices—“educational, not commercial,” he says. In years to come, though, he may get questions about gaining approval from the FDA for Abbott’s ID NOW. The new Covid-19 test was touted at White House briefings as Americans desperately wanted to learn whether they’d been infected without having to enter a hospital, and cities, such as Detroit, wanted to test their police. “I’d never seen the FDA act so quickly,” he says. Next came the challenge of mass production.
Isolating with his wife and two of his three sons while Abbott’s production facility was on lockdown to protect its workers, Moore did have one outing beyond the supermarket. To assure secure procurement of an enzyme needed for the Covid-19 test that was available only at a site in California, he found himself on a plane—then self-quarantined with its pilots while waiting—to collect and bring the enzyme safely back to Maine, where it was put to immediate use.
Daniel J. Skiest ’84
Director, Clinical Research, Division of Infectious Disease, Baystate Health
Springfield, Massachusetts
“Collectively we’ve been warning about a pandemic for years. It was only a question of when and what,” says Skiest, who helped his hospital prepare for the inevitable with a flurry of moves. Policies evolved. Elective surgeries stopped. Patients who arrived in the emergency room with a fever and cough were immediately brought to the back and not left in the waiting area where they could expose others. Only one visitor was allowed per patient, then none. A 30-bed ICU for cardiac patients became a Covid-19 ICU as the number of patients grew from two per day to 20 to 25 per day. An entire hospital wing was devoted to treating the virus.
Most important, he says, are the three-dozen teams the hospital designated to handle Covid-related issues such as employee testing, research, and ethics. Those teams were asked to respond nimbly, changing procedures every couple of days in some cases, as new techniques came to light. For instance, discovering that victims breathe better lying on their stomachs, when their air sacs aren’t as prone to fill with fluids, prompted a new policy. “We are learning as we go along because the literature is coming out daily,” Skiest says. “Everyone is just sort of rolling up their sleeves and doing what they can.”
There has been personal risk. For a few days in March, Skiest thought he might have contracted Covid-19: After seeing about a half-dozen patients, and despite gloves and protective gear, he developed a cold and low-grade fever, prompting a weeklong self-quarantine before he received negative test results that enabled him to return to work. After fear-filled days, Skiest is cautiously optimistic. Testing has become easier. Whereas the hospital used to have to send out tests and wait up to seven days, it now has in-house results in less than a day. Social distancing appears to be working to reduce pressure on hospitals. In March, nearly 60 Covid patients were in intensive care, but by mid-April, when Skiest spoke with DAM, that number had dropped in half: “Everything is becoming a little more manageable,” he says.
Ross E. McKinney Jr. ’75
Chief Scientific Officer
Association of American Medical Colleges
Washington, D.C.
For coronavirus testing to ever meet demand, academic hospital labs must fully engage, McKinney says, noting that the two major private chains in the United States—Quest Diagnostics and LabCorp—can jointly handle only 85,000 tests a day. A former division chief of pediatric infectious diseases at Duke, McKinney now advocates for medical schools by nudging officials to round up the equipment necessary for widespread tests in the schools’ labs.
It hasn’t been easy. As widely reported, special nose swabs needed for tests—with nylon tips, preferably, since cotton can contaminate—have been in drastically short supply, he says, in part because one of the few companies to make them, Capon Diagnostics, is in northern Italy. After McKinney and others called attention to the problem, the U.S. Air Force in March airlifted 1 million swabs from Capon to the United States, an effort that continued through April. “It still is not enough,” McKinney says. In part he blames the FDA for dragging its feet in authorizing alternate sources: “They screwed up.”
Supplies including plastic tubes, protective gear, and RNA extraction kits (the first diagnostic step in sampling the mucus gathered by a swab) are not the only things missing. Many hospitals are short on staff, which has led to calls to enlist medical students to bail out overtaxed emergency rooms, something McKinney argues against. Since “students are learners more than doers” and because they could tie up vital gear, McKinney prefers they provide backup help instead: running day care for children of doctors and nurses, delivering meals to healthcare workers, and checking on patients in isolation by phone.
McKinney’s next challenge will be to train “contact tracers” to interview Covid-19 victims to figure out who has been within 6 feet of them in the past three days. “We’re going to need a small army of contact tracers,” he says, which might be drawn from the ranks of the recently unemployed. “It is such a crisis, such a tsunami, you are grasping at anything to keep yourself afloat.”
Scott Filler ’79
Chief, Division of Infectious Diseases Harbor-UCLA Medical Center
Professor, David Geffen School of Medicine
Torrance, California
Often overlooked in discussions of those at risk of infection from the coronavirus are the homeless, who may live in cramped conditions where self-quarantining is not possible. Many have underlying diseases, too. With one of the largest homeless populations in the country, Los Angeles has been trying to get people off Skid Row and into shelters. By mid-April, the city’s 20 temporary shelters were full—but not every homeless person was off the street.
Filler’s hospital, a public institution that often attracts indigent patients thanks to subsidized care, has seen an influx of homeless patients since the pandemic exploded, though the rate has been lower than expected. “We’re wondering, are they dying on the street?” Filler says. “We’re waiting to see what happens.” Meanwhile, the more marked surge of patients has been from well-to-do communities such as Santa Monica that are served by the hospital. “Wealthier people tend to travel internationally and bring Covid-19 back,” he says.
Regardless, the health crisis has hit the hospital hard. Under normal circumstances Harbor-UCLA would have one medical intensive care team—now it has three. An emergency room has been turned into an ICU to deal with Covid-19 cases.
The hospital, where a couple of doctors were infected with the virus, has carved itself into two camps: one for coronavirus cases, the other for everything else. Ideally, everyone who walks through the door would get a Covid test, but due to a drastic shortage, tests have to be rationed. Nursing home residents, for instance, automatically get one, but there are few guarantees for anyone else. “We’re really hamstrung by a lack of tests,” Filler told DAM in mid-April, though the testing situation improved by the end of the month and he was able to get results for hospitalized patients within a few hours. “You sign up for situations like this.”
Mark Franklin ’98
Critical Care Physician, Dartmouth-Hitchcock Medical Center
Lebanon, New Hampshire
Franklin has worked in DHMC’s intensive care unit since 2008. Starting in 2016, he branched out into telemedicine as the hospital partnered remotely with Sioux Falls, South Dakota-based Avera ecare ICU to explore supporting other area hospitals before launching its own teleICU in July 2019. The hub serves not only DHMC’s 60 adult ICU beds but also hospitals in Bennington, Vermont, as well as Keene and Littleton, New Hampshire, where ICU capabilities are limited. He has colleagues, friends, and many patients—including one who recovered from Covid-19—he has never met in person, only on screen. “A sick patient is a sick patient,” he says.
Practicing telemedicine does have its differences, though: “Initially the toughest adjustment was navigating separate medical records,” says Franklin. Now a Philips eCareManager platform brings records, lab test results, other remote data, and predictive analytics to monitors instantaneously. “Practicing medicine stays the same,” says Franklin, “but telemedicine means working through AV capabilities to build trust and partnerships. You always want to discuss, not dictate.” During the pandemic his biggest challenge, he says, has been getting doctors he knows only virtually “to believe they can go farther than they have gone before and to do things they haven’t done before, because that’s what’s needed.”
After the Covid-19 victim was out of danger, one of the onsite caregivers introduced Franklin to the patient as “the physician who saved your life.” Franklin deflected the accolade. “As I hastened to point out, I was one of many people who treated him, I’d just been on duty a lot,” he says. “But I’ll admit it was nice to hear.”
Daniel B. Klein ’69
Former Chief of Infectious Diseases
Kaiser Permanente San Leandro Medical Center
San Leandro, California
There’s little mincing of words when Klein, who spent his career battling the HIV/AIDS crisis, weighs the federal government’s response to the current pandemic. Although officials were slow to realize the danger posed by HIV, Klein finds the federal response to Covid-19 even worse. “It’s been a clusterf***,” he says. “I don’t know if you can use that word, but it’s really how I feel.”
Klein, who retired last year but hopes to return to work at his old hospital, is more sparing with his criticism of members of the president’s coronavirus task force: Anthony Fauci, the chief resident at Cornell in the early 1970s when Klein was there studying medicine, once memorably drilled Klein about the correct antibiotic to be used for staph infections. Klein gave the wrong answer. (Correct response: methicillin.) “I never forgot that again,” he says.
Completing his training in San Francisco in 1981 as unusual pneumonia was turning up among gay men, Klein found himself working with patients whose level of contagiousness was not initially understood. But the current crisis is worse. “Dedicated people weren’t fearful for their lives while working in hospitals, afraid to come home and infect their families, or putting their wills in order,” he says.
Despite the economic toll from quarantines that have immobilized entire cities, Klein feels the shutdowns were, in terms of public health, warranted. As some leaders called for a May reopening of “nonessential” businesses, Klein favored a more conservative approach, even though doubtful the powers that be will do the right thing. “If it costs trillions of dollars to keep people alive, then we should do it,” he told DAM in April. “A rush to return to normalcy could be a grievous error.”
Illustrations by Joel Kimmel